doi: 10.56294/nds2024120
ORIGINAL
Stress in nurses working in health facilities during the COVID-19 pandemic in North Lima
Estrés en enfermeras que laboran en establecimientos de salud durante la pandemia del COVID-19 en Lima Norte
Rafael Romero-Carazas1 ![]() *, Victor
Cornejo-Aparicio2, Jessica Karina Saavedra-Vasconez3
*, Victor
Cornejo-Aparicio2, Jessica Karina Saavedra-Vasconez3 ![]() , Milagros Andrea Bracho Rivera4
, Milagros Andrea Bracho Rivera4 ![]() *,
Alejandro Carías5
*,
Alejandro Carías5
1Universidad Nacional de Moquegua. Moquegua, Perú.
²Universidad Nacional de San Agustín de Arequipa. Arequipa, Perú.
³Universidad Peruana Unión. Lima, Perú.
⁴Universidad de Panamá. Panamá.
⁵Unidad de Investigación Científica, Facultad de Ciencias Médicas, Universidad Nacional Autónoma de Honduras. Tegucigalpa, Honduras.
Cite as: Romero-Carazas R, Cornejo-Aparicio V, Saavedra-Vasconez JK, Bracho Rivera MA, Carías A. Stress in nurses working in health facilities during the COVID-19 pandemic in North Lima. Nursing Depths Series. 2024; 3:120. https://doi.org/10.56294/nds2024120
Submitted: 02-07-2023 Revised: 01-10-2023 Accepted: 13-01-2024 Published: 15-01-2024
Editor: Dra.
Mileydis Cruz Quevedo ![]()
Corresponding Author: Rafael Romero-Carazas *
ABSTRACT
Work-related stress among nursing professionals is one of the most common problems in their work environment. Factors such as a shortage of biosafety equipment, high patient demand, and inadequate communication among staff significantly increase stress, interfering with the quality of patient care. Therefore, the objective of this research is to determine the stress levels of nurses working in healthcare facilities during the COVID-19 pandemic in northern Lima. This is a quantitative, descriptive, cross-sectional study with a population of 255 nurses who responded to a questionnaire on sociodemographic data and the Spanish version of the Nursing Stress Scale. The results showed that among professionals who have been on duty for 1 to 5 years, 22,4 % have low stress, 43,9 % have medium stress, and 33,6 % have high stress. In conclusion, strategies should be implemented to maintain the mental health of nurses through counseling with professionals specialized in mental health.
Keywords: Stress; Occupational Stress; Nursing Professionals; Mental Health.
RESUMEN
El estrés laboral en los profesionales de enfermería es uno de los problemas más comunes dentro de su entorno laboral, factores como escasez de equipos de bioseguridad, alta demanda de paciente y el no tener una comunicación adecuada entre personal, hace que el estrés aumente considerablemente interfiriendo en una atención de calidad en los pacientes, por tanto el objetivo de investigación es determinar el estrés en enfermeras que laboran en establecimientos de salud durante la pandemia del COVID-19 en Lima Norte. Es un estudio cuantitativo, descriptivo-transversal con una población de 255 enfermeras que respondieron un cuestionario de datos sociodemográficos y el Nursing Stress Scale en su versión español. En los resultados se pudo observar que los profesionales que están de servicio entre 1 a 5 años el 22,4 % tienen estrés bajo, 43,9 % estrés medio y 33,6 % estrés alto. En conclusión, se debe realizar estrategias que permitan mantener la salud mental saludable de las enfermeras a través de consejerías con profesionales especializados en salud mental.
Palabras clave: Estrés; Estrés Laboral; Profesionales de Enfermería; Salud Mental.
INTRODUCTION
Work-related stress is defined as a physical and mental condition that is, in most cases, caused by heavy workloads or overwork, long working hours, or unfavorable conditions in the workplace or organization.(1)
According to the World Health Organization, occupational burnout syndrome is "the result of chronic workplace stress that has not been successfully managed" and clarifies that "it refers specifically to phenomena in the work context and should not be used to describe experiences in other areas of life".(2) In turn, the International Labor Organization (ILO) defines "stress as a physical and emotional response to wear and tear caused by perceived demands on a person and that the result is imposed by the person's capacity, resources, and needs to cope with them."(3)
In this sense, the COVID-19 pandemic has shown that we have an unstable healthcare system, as well as a shortage of nurses to deal with the situation on the front line. Many factors, such as inadequate personal protective equipment, lack of decent working conditions, work procedures that do not meet international standards, and insufficient multidisciplinary and interdisciplinary teams, generate episodes of stress that hinder the work of nursing professionals.(4)
Although there are currently a variety of studies on how the COVID-19 pandemic has caused a great deal of stress on different health systems, this has compromised the workforce, particularly nurses. It is evident that among healthcare professionals, nurses suffer from anxiety and stress due to caring for and treating patients.(5) Given that work-related stress among nurses can affect their quality of life and, at the same time, the quality of care, which is of particular importance, as they can provide more effective services when they have a better quality of life.(6,7)
This global health emergency represents one of the greatest challenges for nursing professionals as members of the healthcare team. The high transmissibility of COVID-19 and the lack of a defined treatment for its control are aspects that affect the psychosocial well-being of nurses. As a result, negative emotions and thoughts can damage their mental health, affecting their performance of tasks related to healthcare, their situational management skills, and the quality of care.(8)
A study in the United States of 3 957 661 nurses revealed that among the reasons why they left their jobs, 31,5 % cited stress as the reason. Among those surveyed who reported leaving or considering leaving their jobs due to burnout, 68,6 % reported a stressful work environment and 63,0 % reported inadequate staffing. This suggests that burnout is a serious problem among US nurses who are quitting or considering doing so. Healthcare systems should focus on implementing known strategies to reduce burnout, including adequate staffing levels for nurses and shorter work shifts.(9)
A study conducted in Mexico on 126 nurses in the context of COVID-19 revealed that 81 % of participants were female, most of whom worked the night shift, 58,7 % reported working 12 hours per day, 44,4 % had 7 or more patients in their care, while 16 % said they had contracted COVID-19. The predominant level of stress was medium, with the main stressors being workload and psychological aspects such as dealing with the death and suffering of their patients.(10)
In Europe, a study conducted in the city of Granada, Spain, revealed that in the intensive care area, nurses experienced work-related stress, with the causal factors being a lack of professionals, a noisy environment, personality, meticulousness, and a lack of staff. The study concluded that intervention programs are needed to help nurses cope with stress, which will greatly improve the quality of care provided to patients.(11) Similarly, in Australia, the incidence of stress and anxiety among nurses was found to be 41,2 %.(12)
In Asia, a study conducted in the city of Tabriz, Iran, on 115 nurses from two hospitals showed that work-related stress has a negative effect on nurses' health-related quality of life, which can overshadow care performance and reduce such behaviors in nurses, which may be one of the factors affecting patient outcomes.(13)
In India, a study found nine factors responsible for occupational stress among nurses in the Indore region, which are monetary and non-monetary evaluation, capacity utilization, time pressure, organizational culture, conflicting demands, work climate, overlapping responsibilities, identification with the organization, and role expectations.(14)
A study conducted in various hospitals and departments specializing in infectious diseases in China involving 1,536 nurses found that 88,2 % experienced an effort-reward imbalance, demonstrating that work stress is negatively correlated with psychological resilience and that psychological resilience is positively correlated with quality of life. This is an indirect effect of work-related stress on quality of life through psychological resilience, indicating that psychological resilience plays a partial mediating role.(15)
In South America, a study conducted in Ecuador on 51 nurses in the city of Riobamba revealed that the prevalence of work-related stress was 84,51 %, with nursing staff suffering greater exposure to work-related stress. This demonstrated that the most exposed dimension was cohesion, with a significant negative correlation being identified between work-related stress and self-perceived health.(16)
In Peru, a study of 126 nursing professionals in the emergency services of two level III public hospitals in Lima and Callao revealed that 39,1 % of nurses presented some degree of anxiety, 24,6 % some degree of depression, and 8,8 % some degree of stress. Nurses who care for patients suspected of having COVID-19 in emergency services experience higher levels of anxiety than depression, and in a few cases, they experience stress.(17)
Therefore, the objective of the research is to determine the stress levels of nurses working in healthcare facilities during the COVID-19 pandemic in northern Lima.
METHOD
Research type and design
The research is quantitative in nature, using a descriptive-cross-sectional, non-experimental methodology.(18)
Population
The population consists of a total of 255 nursing professionals working in a health facility.
Inclusion Criteria
· Nursing professionals who have been working at the health facility for more than one year.
· Nursing professionals who only work in a hospital setting
· Nursing professionals who voluntarily agree to participate.
Technique and Instrument
The data collection technique used was a survey, providing sociodemographic information and the Nursing Stress Scale (NSS) instrument by Gray et al.(19) ; however, for the research work, the version validated in Spanish by Más et al.(20).
The NSS instrument comprises 34 items divided into three dimensions (physical environment, psychological environment, and social environment), which are assessed using a Likert scale with four response options: "0 = Never," "1 = Sometimes," "2 = Frequently," and "3 = Very frequently," which yields a total score of 0 to 102 points, distributed into three levels: low, medium, and high. The higher the score, the higher the level of stress among nursing professionals.
The instrument was validated using the Kaiser-Mayer-Olkin sample adequacy test, with a result of 0,950 (KMO > 0,6), while Bartlett's sphericity test yielded significant results (X2approx. = 6241,645; gl = 561; p = 0,000).
Finally, the reliability of the instrument was determined using Cronbach's alpha, obtaining a result of 0,962 (α > 0,8).
Place and Application of the Instrument
The instrument was applied after prior coordination with each of the nursing professionals participating in the study, in addition to providing them with information about the study to be conducted.
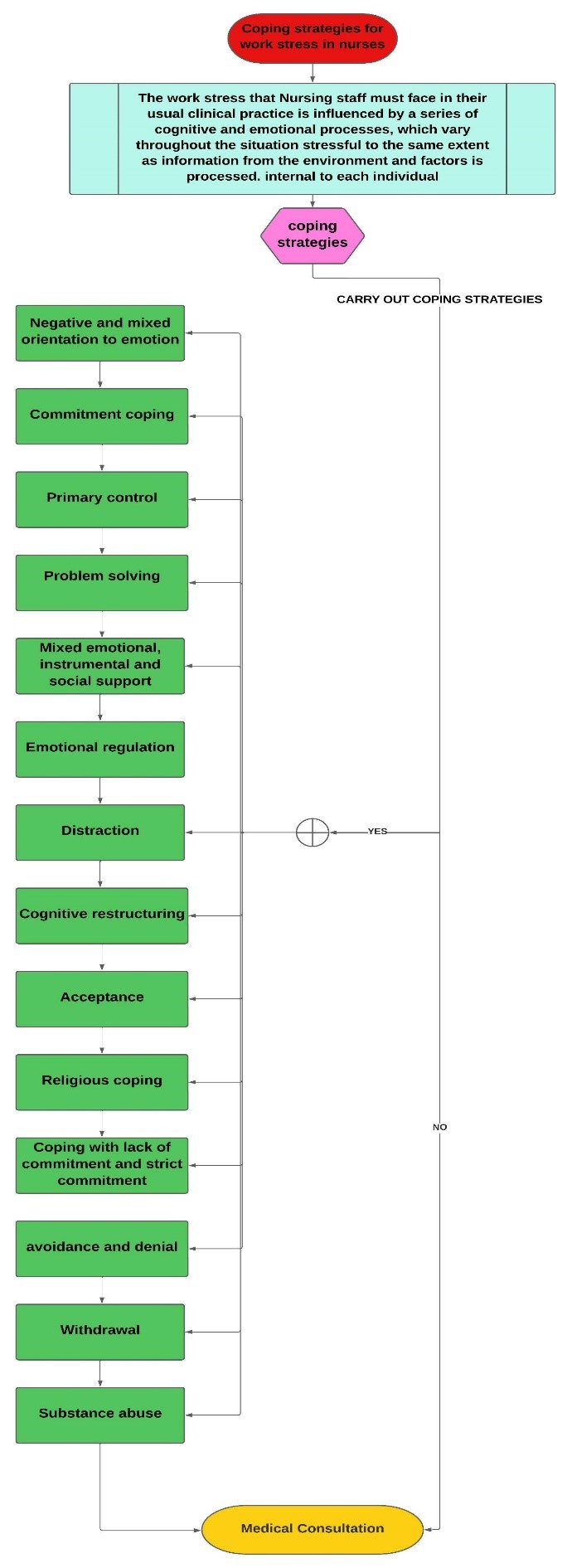
Figure 1. Flowchart of coping strategies used by nurses in situations that cause work-related stress
This flowchart shows the strategies that nursing professionals can use when faced with stressful situations in the workplace.
The coping strategies chosen by nursing professionals are adapted to work-related stress, as they constitute an important personal resource, in which clinical intervention is carried out both individually and in groups. As these are factors that can be modified through interventions that improve coping strategies, this will enable nursing professionals to minimize the consequences of work-related stress.
However, not all coping styles are beneficial for nursing professionals, as some personal coping styles not only fail to reduce work-related stress but can actually increase it if not managed correctly.
Therefore, both hospital and community centers should promote all types of interventions and programs that allow for the development or improvement of coping strategies that are adaptable to work-related stress, so that nurses can cope with stressful situations in their work environment, with the aim of improving their routine nursing practice.
RESULTS
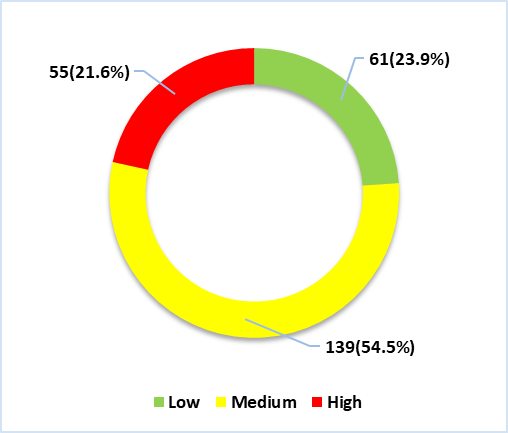
Figure 2. Stress in nurses working in healthcare facilities during the COVID-19 pandemic in Northern Lima
In figure 2, we can see that 23,9 % (n=61) of participants have low stress levels, 54,5 % (n=139) have medium stress levels, and 21,6 % (n=55) have high stress levels.
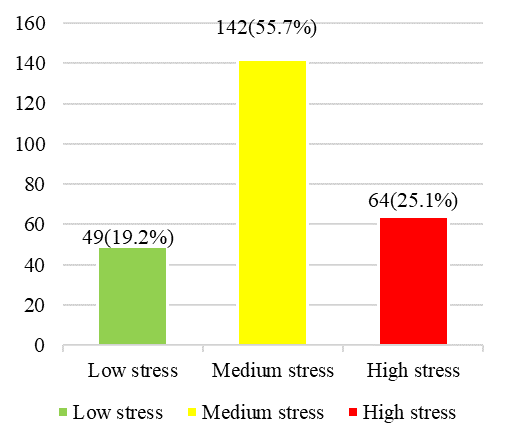
Figure 3. Stress among nurses in terms of their physical environment working in healthcare facilities during the COVID-19 pandemic in northern Lima
Figure 3 shows that 19,2 % (n=49) of participants have low stress levels with regard to the physical environment dimension of stress, 55,7 % (n=142) have medium stress levels, and 25,1 % (n=64) have high stress levels.
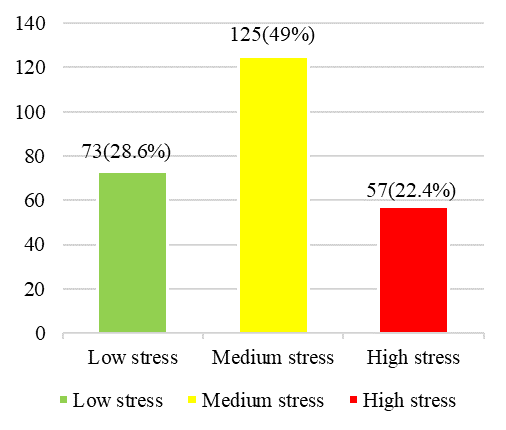
Figure 4. Stress among nurses in terms of their psychological environment working in healthcare facilities during the COVID-19 pandemic in northern Lima
In figure 4, we can see that 28,6 % (n=73) of participants have low stress levels with regard to their psychological environment, 49 % (n=125) have medium stress levels, and 22,4 % (n=57) have high stress levels.
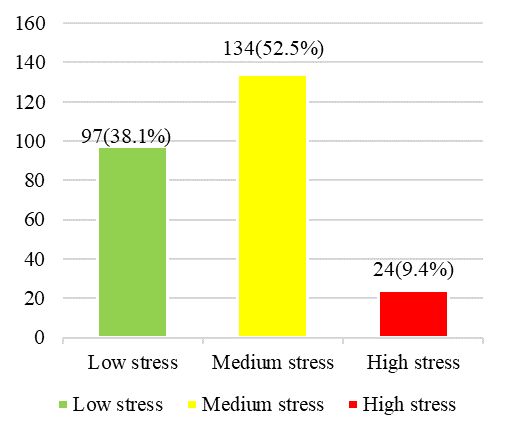
Figure 5. Stress in nurses in their social environment dimension working in health facilities during the COVID-19 pandemic in Northern Lima
In figure 5, we can see that 38,1 % (n=97) of participants have low stress levels with regard to their social environment, 52,5 % (n=134) have medium stress levels, and 9,4 % (n=24) have high stress levels.
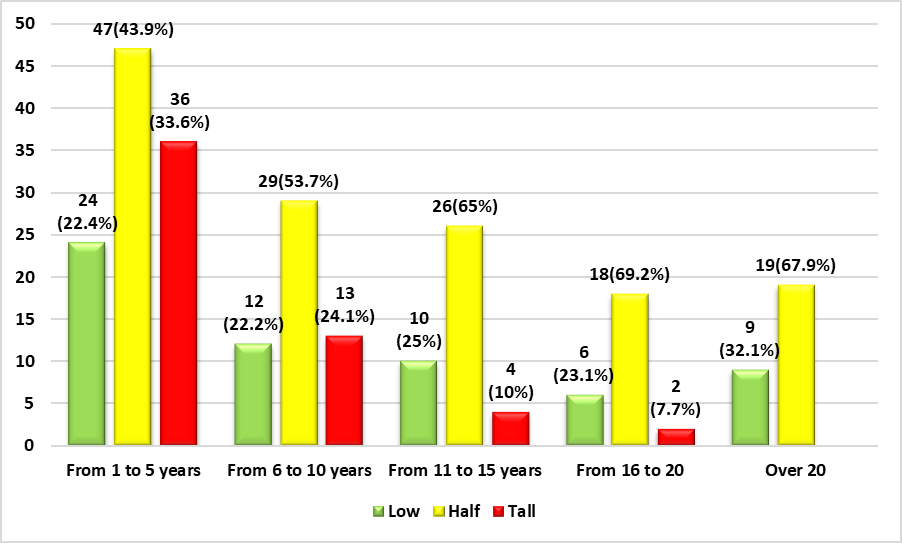
Figure 6. Stress among nurses in relation to their years of service working in healthcare facilities during the COVID-19 pandemic in Northern Lima
In figure 6, we can see that 22,4 % (n=24) of participants who have been in service for 1 to 5 years have a low level, 43,9 % (n=47) have a medium level, and 33,6 % (n=36) have a high level. Among participants who have been in service for 6 to 10 years, 22,2 % (n=12) of participants have a low level of stress, 53,7 % (n=29) have a medium level, and 24,1 % (n=13) have a high level of stress. As for participants who have been in service for 11 to 15 years, 25 % (n=10) have a low level of stress, 65 % (n=26) have a medium level of stress, and 10 % (n=4) have a high level of stress. Among participants who have been in service for 16 to 20 years, 23,1 % (n=6) have a low level of stress, 69,2 % (n=18) have a medium level of stress, and 7,7 % (n=2) have a high level of stress. As for participants who have been in service for more than 20 years, 32,1 % (n=9) have low stress levels and 67,9 % (n=19) have medium stress levels.
DISCUSSIONS
This research is presented from the perspective of promoting and preventing work-related stress among nursing professionals, given that stress is on the rise. For this reason, coping strategies were developed to minimize stressful situations among nursing professionals.
The results of the main variable, work-related stress, show that healthcare professionals have a medium level of work-related stress. This is because the mental health of nursing professionals was compromised during the COVID-19 pandemic, where factors such as excessive workload, high patient demand, extra shifts at work, lack of communication at work, and a shortage of human resources increased stress levels. As a result, nursing professionals tend to experience work-related stress, making them more vulnerable to mental disorders.
In the results of the different dimensions, we can see that nursing professionals have medium job stress in terms of physical, psychological, and social dimensions. This is because nursing professionals are committed to both their mental and physical well-being, which leads to factors such as exhaustion and work overload, indicating that they are mentally stressed about their work, given that the work environment in which they work is stressful. The pressure exerted on them at work has consequences that hinder their ability to adapt to the work environment, which in turn leads to increased levels of stress at work.
In terms of the results of the work experience, we can observe that workers with less than 5 years of experience tend to report higher levels of stress, given that, as they are new to caring for COVID-19 patients, they are vulnerable to symptoms of stress, as they use advanced resources to care for COVID-19 patients, and without sufficient guidance, the high demand for patients will be a major challenge for these workers, making them more susceptible to stress at work.
CONCLUSIONS
It is concluded that strategies should be promoted to maintain the mental health of nursing professionals by providing counseling through mental health professionals.
It is concluded that strategies should be promoted to enable nursing professionals to cope with any situation that causes stress in the workplace.
It is concluded that educational talks on stress and methods to prevent it should be held in the work environment of nursing professionals.
BIBLIOGRAPHIC REFERENCES
1. E. Kakeman, P. Raeissi, S. Raoofi, A. Soltani, M. Sokhanvar, and D. Visentin, “Occupational stress and associated risk factors among nurses: a cross-sectional study,” Contemp. Nurse, vol. 55, no. 3, pp. 237–249, 2019, doi: 10.1080/10376178.2019.1647791?scroll=top.
2. Organización Panamericana de la Salud, “Estrés laboral es una carga para los individuos, los trabajadores y las sociedades,” OPS, 2020. https://www3.paho.org/hq/index.php?option=com_content&view=article&id=11973:workplace-stress-takes-a-toll-on-individuals-employers-and-societies&Itemid=0&lang=es#gsc.tab=0
3. Organización Internacional del Trabajo, “Estrés en el trabajo : un reto colectivo,” OIT, 2016. https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---safework/documents/publication/wcms_466549.pdf
4. S. Cassiani, E. Munar, A. Umpiérrez, M. Peduzzi, and C. Leija, “La situación de la enfermería en el mundo y la Región de las Américas en tiempos de la pandemia de COVID-19,” Rev. Panam. Salud Publica/Pan Am. J. Public Heal., vol. 44, no. 1, p. e64, 2020, doi: 10.26633/RPSP.2020.64.
5. J. De los Santos and L. Labrague, “Impact of COVID-19 on the Psychological Well-Being and Turnover Intentions of Frontline Nurses in the Community: A Cross-Sectional Study in the Philippines,” medRxiv, vol. 1, no. 1, pp. 1–27, 2020, doi: 10.1101/2020.08.05.20167411.
6. I. Layali, M. Ghajar, E. Abedini, S. Emadian, and M. Joulaei, “Role of Job Stressors on Quality of Life in Nurses,” J. Manzadaran Univ. Med. Sci., vol. 29, no. 180, pp. 129–133, 2019, Accessed: Nov. 05, 2022. https://jmums.mazums.ac.ir/article-1-12238-en.pdf.
7. B. Meneses, N. Gonzalez, W. Alvarado, and J. Meneses, “Stress in nursing professionals who work in the first line of care against covid – 19 in north lima,” J. Med. Pharm. Allied Sci., vol. 10, no. 6, pp. 3937–3941, 2021, doi: 10.22270/JMPAS.V10I6.1732.
8. I. Ricci et al., “Impact of viral epidemic Outbreaks on mental health of healthcare workers: A rapid systematic review,” Med Rxiv, vol. 4, no. 6, pp. 1–92, 2020, doi: 10.1101/2020.04.02.20048892.
9. M. Shah, N. Gandrakota, J. Cimiotti, N. Ghose, M. Moore, and M. Ali, “Prevalence of and Factors Associated with Nurse Burnout in the US,” JAMA Netw. Open, vol. 4, no. 2, pp. 1–11, Feb. 2021, doi: 10.1001/jamanetworkopen.2020.36469.
10. P. García, A. Jiménez, L. Hinojosa, G. Gracia, L. Cano, and A. Abeldaño, “Estrés laboral en enfermeras de un Hospital Público de la zona fronteriza de México, en el contexto de la pandemia COVID-19,” Rev. Salud Publica, vol. 1, no. 1, pp. 65–73, 2020, doi: 10.31052/1853.1180.
11. G. Cobos, A. Soriano, and M. Seijo, “Estrés laboral en Enfermería de Cuidados Críticos,” SANUM Rev. Cient. Sanit., vol. 5, no. 4, pp. 74–85, 2021, Accessed: Nov. 05, 2022. https://www.revistacientificasanum.com/pdf/sanum_v5_n4_a9.pdf.
12. S. Maharaj, T. Lees, and S. Lal, “Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses,” Int. J. Environ. Res. Public Health, vol. 16, no. 1, pp. 1–10, Jan. 2019, doi: 10.3390/ijerph16010061.
13. A. Reza, N. Gahassab, and A. Fathnezhad, “Nurses’ job stress and its impact on quality of life and caring behaviors: a cross-sectional study,” BMC Nurs., vol. 21, no. 1, pp. 1–10, Dec. 2022, doi: 10.1186/s12912-022-00852-y.
14. A. Veda and R. Roy, “Occupational Stress Among Nurses: A Factorial Study with Special Reference to Indore City,” J. Health Manag., vol. 22, no. 1, pp. 67–77, Mar. 2020, doi: 10.1177/0972063420908392.
15. J. Yan, C. Wu, Y. Du, S. He, L. Shang, and H. Lang, “Occupational Stress and the Quality of Life of Nurses in Infectious Disease Departments in China: The Mediating Role of Psychological Resilience,” Front. Psychol., vol. 13, no. 1, pp. 1–11, Mar. 2022, doi: 10.3389/fpsyg.2022.817639.
16. J. Lucero, D. Noroña, and V. Vega, “Estrés laboral y autopercepción de la salud en médicos y enfermeras del área de emergencia en Riobamba, Ecuador,” Rev. Cuba. Reumatol., vol. 23, no. 1, pp. 1–17, 2020, Accessed: Nov. 05, 2022. http://www.revreumatologia.sld.cu/index.php/reumatologia/article/view/945/pdf_1.
17. R. Obando, J. Arevalo, R. Aliaga, and M. Obando, “Ansiedad, estrés y depresión en enfermeros de emergencia Covid-19,” Index de Enfermería, vol. 29, no. 4, pp. 1–9, 2021, Accessed: Nov. 05, 2022. https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1132-12962020000300008.
18. C. Fernández and P. Baptista, “Metodología de la Investigación.” p. 634, 2015, http://observatorio.epacartagena.gov.co/wp-content/uploads/2017/08/metodologia-de-la-investigacion-sexta-edicion.compressed.pdf.
19. R. Más and V. Escribá, “La Versión Castellana de la Escala ‘The Nursing Stress Scale’. Proceso de Adaptación Transcultural,” Rev Esp Salud Pública, vol. 72, no. 1, pp. 529–538, 1998, https://scielo.isciii.es/pdf/resp/v72n6/castellana.pdf.
20. P. Gray and J. Anderson, “The Nursing Stress Scale: Development of an instrument,” J. Behav. Assess., vol. 3, no. 1, pp. 11–23, 1981, doi: 10.1007/BF01321348.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Rafael Romero-Carazas, Victor Cornejo-Aparicio, Jessica Karina Saavedra-Vasconez, Milagros Andrea Bracho Rivera, Alejandro Carías.
Data curation: Rafael Romero-Carazas, Victor Cornejo-Aparicio, Jessica Karina Saavedra-Vasconez, Milagros Andrea Bracho Rivera, Alejandro Carías.
Formal analysis: Rafael Romero-Carazas, Victor Cornejo-Aparicio, Jessica Karina Saavedra-Vasconez, Milagros Andrea Bracho Rivera, Alejandro Carías.
Drafting - original draft: Rafael Romero-Carazas, Victor Cornejo-Aparicio, Jessica Karina Saavedra-Vasconez, Milagros Andrea Bracho Rivera, Alejandro Carías.
Writing - proofreading and editing: Rafael Romero-Carazas, Victor Cornejo-Aparicio, Jessica Karina Saavedra-Vasconez, Milagros Andrea Bracho Rivera, Alejandro Carías.