doi: 10.56294/nds202361
ORIGINAL
The role of nursing in patients with postpartum haemorrhage
Rol de enfermería en pacientes con hemorragia postparto
Bryan Enrique Jarrin Valarezo1, Joselyn Katherine Arias Olmedo1, Kathiusca Paola Echeverría Caicedo1
1Universidad Estatal De Milagro, Facultad De Salud Y Servicios Sociales, Licenciatura En Enfermería. Milagros, Ecuador.
Cite as: Jarrin Valarezo BE, Arias Olmedo JK, Echeverría Caicedo KP. The role of nursing in patients with postpartum haemorrhage. Nursing Depths Series. 2023; 2:61. https://doi.org/10.56294/nds202361
Submitted: 01-05-2022 Revised: 15-09-2022 Accepted: 01-01-2023 Published: 02-01-2023
Editor: Dra.
Mileydis
Cruz Quevedo ![]()
ABSTRACT
The research focused on analysing the role of nursing professionals in dealing with postpartum haemorrhage, one of the leading causes of maternal mortality worldwide and the second leading cause in Ecuador. This study, which was documentary and bibliographic in nature and used a quantitative approach, identified the importance of nursing staff in the prevention, detection and management of this obstetric emergency. It was highlighted that, among their duties, the care and educational roles were the most relevant. In the care area, staff performed interventions such as assessing vital signs, administering uterotonic drugs, transfusions and uterine massage. In their educational role, they provided guidance to patients and family members on warning signs and self-care measures. Likewise, a knowledge deficit was evident among some health personnel and patients, which affects the effective response to these emergencies. The use of the Nursing Care Process (NCP) was identified as a fundamental tool for planning, executing, and evaluating care in a structured and effective manner. The main cause of postpartum haemorrhage was uterine atony, which was responsible for 70 % of cases. Finally, it was recommended that ongoing training for nursing staff be strengthened and that the Ministry of Health’s Clinical Guidelines be followed to improve the quality of care and reduce maternal morbidity and mortality.
Keywords: Postpartum Haemorrhage; Nursing Role; Primary Care; Uterine Atony; Prevention.
RESUMEN
La investigación se centró en analizar el rol del profesional de enfermería frente a las hemorragias postparto, una de las principales causas de mortalidad materna a nivel mundial y la segunda en Ecuador. Este estudio, de tipo documental bibliográfico y enfoque cuantitativo, permitió identificar la importancia del personal de enfermería en la prevención, detección y manejo de esta emergencia obstétrica. Se destacó que, dentro de sus funciones, los roles asistencial y educativo fueron los más relevantes. En el ámbito asistencial, el personal realizó intervenciones como la valoración de signos vitales, administración de fármacos uterotónicos, transfusiones y masajes uterinos. En el rol educativo, brindó orientación a las pacientes y familiares sobre signos de alarma y medidas de autocuidado. Asimismo, se evidenció un déficit de conocimientos en parte del personal de salud y de las pacientes, lo cual afecta la respuesta efectiva ante estas emergencias. El uso del Proceso de Atención de Enfermería (PAE) fue señalado como una herramienta fundamental para planificar, ejecutar y evaluar los cuidados de manera estructurada y eficaz. La principal causa identificada de hemorragia postparto fue la atonía uterina, responsable del 70 % de los casos. Finalmente, se recomendó fortalecer la capacitación continua del personal de enfermería y seguir las Guías Clínicas del Ministerio de Salud para mejorar la calidad de atención y reducir la morbimortalidad materna.
Palabras clave: Hemorragia Postparto; Rol de Enfermería; Atención Primaria; Atonía Uterina; Prevención.
INTRODUCTION
Nursing professionals are responsible for performing their roles and providing adequate care, initiating preventive and health promotion actions at different stages of life, regardless of whether people are sick or healthy, making their role substantial in primary care. They are also responsible for remedying the problems of individuals, families, and communities. To provide essential information to help people adopt a healthy lifestyle. Self-care is a fundamental and proactive approach that each person should adopt voluntarily to maintain their health, well-being, and overall progress.(1,2,3)
In cases of postpartum hemorrhage, nursing professionals perform various functions, among which the care and educational roles are most notable. In terms of care, they assist, such as taking or monitoring vital signs, keeping the patient at rest, checking the type of hemorrhage, administering fluids as prescribed by the doctor, administering red blood cells if required, assessing the patient's progress during each shift, and providing emotional support to the patient and their family members. Similarly, in the educational role, activities such as educating the patient and family members about the causes and circumstances of postpartum hemorrhage are carried out.(2,4,5,6)
Postpartum hemorrhage is the loss of any amount of blood that causes instability in the human body. It is also considered a global obstetric emergency, causing morbidity in some cases and maternal death in others. It is therefore necessary for nursing staff to acquire and update their knowledge of the treatment to be given in cases where a patient presents this condition.(3,7,8,9)
The World Health Organization (WHO) reports that postpartum complications are the leading cause of preventable and treatable maternal morbidity and mortality. It is worth noting the reduction in mortality rates in patients who underwent institutional delivery, and it is also considered essential that health services provide more effective, adequate, and readily available support at all levels of care.(4,10,11,12)
Various types of information are currently available, and studies indicate that it is essential to provide health education and adequate knowledge to patients and their families, as well as to strengthen the activities of health personnel to prevent complications from postpartum hemorrhage.
This research is a literature review aimed at summarizing existing knowledge about postpartum hemorrhage and highlighting the symptoms, signs, and behaviors associated with this condition. It also highlights the importance of effective and appropriate nursing care in reducing the condition and preventing various health complications.
Research problem
Problem statement
Human activity is considered a skill of caring, encompassing various actions aimed at maintaining health, as it is essential for people's lives, dedicated to themselves and their behavior, which is necessary to achieve a high degree of independence in health knowledge. Nursing is closely related to a person's past routines, culture, and life. It is also the interaction of values, beliefs, and skills inherited from the past, which, when possible, converge to meet the needs of the people involved in the relationship.(5,13,14,15)
The Nursing Care Process (NCP). This helps professionals refine their care methods and assess changes in patient outcomes. This process involves a series of activities carried out by nursing staff to guide healthy individuals in maintaining a balance with the environment and restoring health to patients. The NCP is suitable for users, families of hospitalized patients, and communities, enabling the healthcare team to participate in rehabilitation alongside family members.(6,16,17,18)
Postpartum hemorrhage is one of the leading causes of maternal morbidity and mortality worldwide, with approximately 14 million pregnant women giving birth each year and 125 000 dying. This highlights the importance of closely monitoring the vital signs of patients with this obstetric emergency to determine the necessary nursing strategies and care. Postpartum hemorrhage occurs when there is a blood loss of more than 500 ml. This bleeding sometimes occurs in the first hours after delivery and is considered the leading cause of maternal death worldwide, with an incidence of 17-40 %.(7,19,20,21)
In Latin America, it is estimated that 8,2 % of women who give birth suffer postpartum hemorrhage that even requires a transfusion. It is considered one of the leading causes of maternal death in Latin America, which is why it is necessary to implement better clinical safety in the care of this obstetric pathology.(8,22,23,24)
In Ecuador, postpartum hemorrhage (PPH) is considered the second leading cause of death in women. According to the Clinical Practice Guidelines for Prevention, Diagnosis, and Treatment. The most common causes of this condition are uterine atony (70 %), cervical injury (20 %), followed by retained placenta or clots (10 %), and finally, pre-existing coagulation (<1 %).(9,25,26,27)
In 2019, the province of Guayas saw a higher number of maternal deaths due to obstetric hemorrhages and other complications, with a total of 70 maternal deaths; on the other hand, in 2020, there was a decrease to 45 maternal deaths. The Ministry of Public Health (MSP) states that uterine atony is one of the most common causes of postpartum hemorrhage. Uterotonic drugs are used as a preventive measure; the most widely recognized are oxytocin and carbetocin. Ergometrine is also used, but it is contraindicated in hypertensive patients.(10,28,29,30)
Postpartum hemorrhage occurs for various reasons that affect women's health after giving birth. When the uterus does not contract with sufficient force, it causes bleeding in the blood vessels. It can also cause tearing of the cervix, tearing of blood vessels, coagulation difficulties, and problems with the placenta.
Similarly, other difficulties can be mentioned, such as uterine atony, which is responsible for causing between 80-90 % of postpartum hemorrhages. On the other hand, we also face the issue of patients' lack of interest in attending their monthly checkups. Insufficient promotion and prevention programs within health institutions lead to a lack of awareness of the risk factors that can cause this condition, resulting in poor self-care and neglect of preventive methods for high-risk pregnancies that can lead to PPH.
Another difficulty that can be noted is tearing of the birth canal, where health professionals in the expulsion phase must act according to the obstetric guidelines established in the manuals and clinical practice guidelines issued by the Ministry of Public Health. On the other hand, there is a lack of updated knowledge among health personnel, as well as among patients and their families.(11,31,32,33)
The high rate of postpartum hemorrhage makes this condition one of the three leading causes of maternal mortality. For this reason, prevention methods are essential to reduce these cases, and this is where the importance of applying the nursing role appropriately lies, allowing measures to be taken to improve health status by strengthening nursing care from the primary level of healthcare.(12,34,35,36)
At the first level of health care, nursing professionals fulfill their duties of disease prevention and health promotion in postpartum hemorrhage, also considered a condition that can be prevented through pharmacological treatment, where these health professionals are responsible for administering the appropriate dose and medication so that women maintain proper health and well-being, together with their families and the entire community.(13,37,38,39)
Prevention is based on uterotonic drugs such as oxytocin, which, due to its half-life, must be administered intravenously for 4-6 hours. The protocol for the prevention of postpartum hemorrhage excludes early clamping of the umbilical cord, as well as uterine massage in women who have received prophylactic oxytocin.(14,40,41,42)
Nursing professionals must be responsible for providing education and care, establishing various self-care methods to enhance the quality of life for a community, including pregnant women, and thereby reducing the incidence of postpartum hemorrhage in different healthcare settings.
The role of nursing in postpartum hemorrhage is that of the health professional who is in direct contact with the patient during the postpartum period. They are responsible for monitoring the patient and observing any possible difficulties, as well as detecting and managing this pathology. Their primary role is to provide care, offering the appropriate treatment when postpartum hemorrhage occurs.(15,43,44,45)
On the other hand, the educational role is responsible for providing pregnant women with knowledge about how postpartum hemorrhage occurs. This information is typically provided after delivery to address any questions patients may have, making the educational role a primary function of nurses in imparting knowledge about their illness. It can be deduced that postpartum hemorrhage can occur in any pregnancy, whether by cesarean section or standard delivery.(46,47,48) In general, prevention and adequate care by nursing professionals should focus not only on the competence of the care role, but also on the importance of educating the patient and her family for the benefit of her health.(16,49,50,51)
It is essential to highlight the role of nursing both in public health and in the hospital setting, promoting the application of humanistic care to patients in labor,(52,53,54,55) bearing in mind that the nursing care process (NCP) is the appropriate tool for providing the respective care to the patient, family, and community.(14,56,57,58)
In response to the current issue, this bibliographic research has been conducted to examine the role of nursing in patients with postpartum hemorrhage, aiming to reduce the problem and establish interventions that can be implemented either immediately or in the long term. To resolve the health problems encountered, the following question is posed:
What is the importance of the nursing role in the prevention and care of postpartum hemorrhage?
General Objective
Analyze the role of nursing in patients with postpartum hemorrhage.
METHOD
This study, entitled "The role of nursing in patients with postpartum hemorrhage," is a bibliographic documentary research with a quantitative approach based on analytical and deductive methods.
This research examines the various roles that healthcare personnel play in managing postpartum hemorrhage. This condition is considered a problem that is part of the morbidity and mortality that is most prevalent in the maternal population, which is currently considered a global health problem. Despite numerous actions and activities undertaken to reduce the prevalence of this issue, it remains prevalent to date. In correlation with this, the WHO reveals that, regardless of the progress made in recent years in reducing the number of women who suffer mortality or morbidity due to postpartum hemorrhage, it continues to be the most common direct cause of maternal death in low-income countries.(17)
Type of research
This is a bibliographic documentary research study. This type of work involves consulting electronic and physical documents, employing a similar approach planned by the researcher to collect as much information as possible related to the research topic, thereby fulfilling the set objectives. This type of research proposes that the researcher outline their ideas and conceptions of the subject under investigation in order to develop new knowledge through reflection and analysis, thereby transforming the researcher into an active and participatory agent about what is being investigated.(18)
Research approach
This research is developed using a quantitative approach. This approach can be used to conduct research, as it enables the definition of all the conceptual points of utmost importance for the discernment of the research. Furthermore, the quantitative approach utilizes statistical data to reveal the reality of an existing problem, using figures to highlight the characteristics that make a problem or topic the subject of research.(19)
Method
The type of method used is deductive. In academic terms, this means extracting. This method emphasizes the application of analysis and reasoning, enabling us to begin with general facts about a topic and progress to specific principles to establish the effectiveness of the research work.(19)
In the current research work, an exhaustive search of bibliographic references related to the topic was conducted, spanning from global to national and local levels. This information was equivalent to that proposed, allowing the objectives formulated to be met.
Sources of information
The primary sources of information were found on the internet. A search for information was conducted on websites related to health, such as the Pan American Health Organization (PAHO), the World Health Organization (WHO), the Ecuadorian Ministry of Public Health (MSP), the Free Maternity Law, Practical Clinical Guide to Postpartum Hemorrhage, as well as various articles from online journals such as SciELO, Redalyc, Dialnet, among others.
Materials
For the storage and processing of information, laptops and desktop computers without a Windows operating system were used. Microsoft Word was used to develop the work. References and bibliographic citations were made using the Mendeley bibliographic manager, version 1.19.8, following APA 6th Edition guidelines.
RESULTS
It is impossible to determine whether nursing staff are up to date with information on patients who suffer postpartum hemorrhage, as this is a condition that causes complications worldwide, depending on the predisposing conditions of different population groups. According to statistical data, this condition affects 2 % of the postpartum female population, which is equivalent to 25 % of all maternal deaths worldwide each year. It is estimated that around 125 000 women die from this obstetric complication, which is considered the leading cause of death in developed and developing countries. The leading cause of postpartum hemorrhage is uterine atony, which occurs in 70 % of cases.(20)
In 2019, in Peru, research conducted by Sandra Mocarro and colleagues sought to determine the risk factors associated with postpartum hemorrhage at the Hospital de la Amistad Perú Corea II2- Santa Rosa de Piura, where, through a careful review of medical records of 338 patients diagnosed with postpartum hemorrhage who had been treated at this hospital, obtained the following results and reached the following conclusions:
Fourteen types of risk factors are associated with postpartum hemorrhage. By looking at figure 1, you can see that the factors are listed in descending order according to their intensity. The boxes in the contingency tables have figures greater than 5, giving greater certainty to the p-value < 0,05. Likewise, among the different types of risk factors for postpartum hemorrhage, we found the following: vaginal tears in 110 patients, representing 65 % of the total; incomplete delivery in 47 patients, representing 28 % of the total; patients with episiotomy in 28. 30 % of whom presented postpartum hemorrhage, while on the other hand, without episiotomy, 60,9 % presented postpartum hemorrhage, and atony/hypotonia were 16 patients, representing 9 %. It is estimated that the leading risk factor for PPH is tearing, with a total of 110 cases, and other causes are shown in figure 1 below.(21)
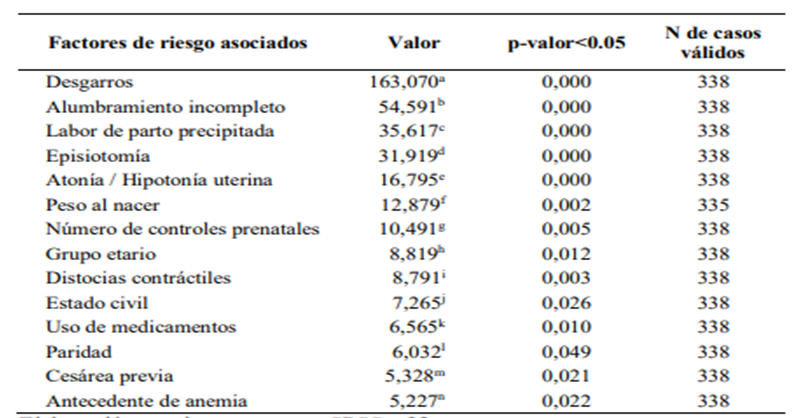
Source: Sandra(21)
Figure 1. Risk factors for postpartum hemorrhage
A study conducted at the Puyo General Hospital (Mexico) in 2021, taking into account a population of 60 women with uterine atony and 13 nursing professionals, for a total of 73, considering as the primary source the patients' medical records and the nursing staff's knowledge of this obstetric pathology, the authors, Master Nairovys Gómez and collaborators, express the following results and conclusions:
Sixty-two percent of the nurses surveyed were unaware of the interventions that should be performed in cases where a patient presents postpartum hemorrhage due to uterine atony, as they mentioned that the first step in care is to administer drugs and perform a blood transfusion. On the other hand, 38 % do know the subject with certainty, mentioning that it is first necessary to assess the woman's level of bleeding, as shown in figure 2.(22)

Source: Gómez et al.(22)
Figure 2. First step in caring for a woman with postpartum hemorrhage due to uterine atony
On the other hand, in the study entitled "Factors associated with obstetric hemorrhage in the immediate postpartum period" conducted at the Juan Bruno Zayas Hospital (Cuba), based on a review from January 2015 to December 2018 in a sample of 105 postpartum women, considering the individual medical records of each patient as the primary source of data, the authors, Dr. Margarita Malpartida Ampudia and collaborators, established the following results and conclusions:
The management and use of oxytocin to induce labor is used in a total of 84,7 % of cases. In comparison, uterine distension is performed in 44,7 % of cases, which are considered in this study to be the main risk factors associated with immediate postpartum hemorrhage. On the other hand, the main etiologies are uterine atony with 35,2 %, soft birth canal injuries with 35,2 %, and retention of ovular membranes with 14,2 %. The results can be seen below in figure 3.(23)
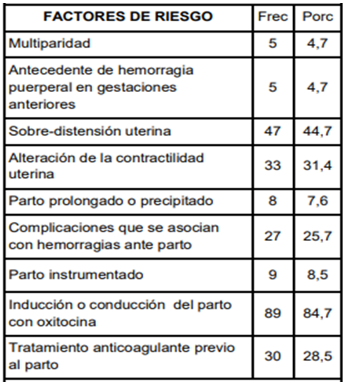
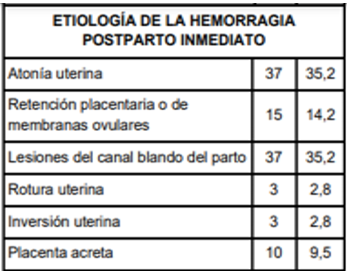
Source: Margarita et al.(23)
Figure 3. Risk factors and etiology of immediate postpartum hemorrhage
Uterine atony remains the primary etiology of obstetric hemorrhage in the immediate postpartum period, so the use of uterotonic drugs is justified as first-line treatment for immediate postpartum hemorrhage.
In the city of Xalapa (Mexico), a research study conducted at the CAE Dr. Rafael Lucio High Specialty Center, which had a population of 12 nurses working in the CAE's obstetric surgery area, concluded that:
There were a total of 12 nurses, representing 100 % of the sample, with 83 % female and 17 % male. The nursing staff's interventions are reflected in the results, as the personnel in charge of the service are aware of the care they must provide to a postpartum patient. All of the nursing staff confirmed that the procedures to detect possible postpartum hemorrhage must be performed; however, they are not performed 100 % of the time.(8)
In a bibliographic study conducted in 2020 by Lic. Graciela Rivera and her participants in the city of Riobamba, Ecuador, which sought to determine the nursing interventions that health personnel should carry out if a patient presents postpartum hemorrhage due to uterine atony, In this study, Hernández Morales MA and García de la Torre J., in their article entitled "Risk Factors for Obstetric Hemorrhage," indicate that the risk factors for this obstetric pathology are being over 25 or under 35 years of age, and patients weighing more than 70 kg have a 60 % chance of developing PPH.(24)
In the city of Guayaquil (Ecuador), in 2020, research was presented by Emily Orrala and Cesar Figueroa at the Guasmo Sur General Hospital entitled "Nursing Care in Patients with Postpartum Hemorrhage in the Gynecology and Obstetrics Emergency Department." The study population consisted of 30 registered nurses who work on a rotating basis in the obstetric emergency department of the aforementioned hospital. This research group commented that:
When faced with a patient with postpartum hemorrhage, as shown in figure 4, 47 % of nursing staff sometimes perform uterine massage every 15 minutes, while 40 % stated that they rarely perform this procedure. Therefore, only 13 % of nursing staff use this method as a preventive measure to reduce the effects of blood loss after childbirth.(25)
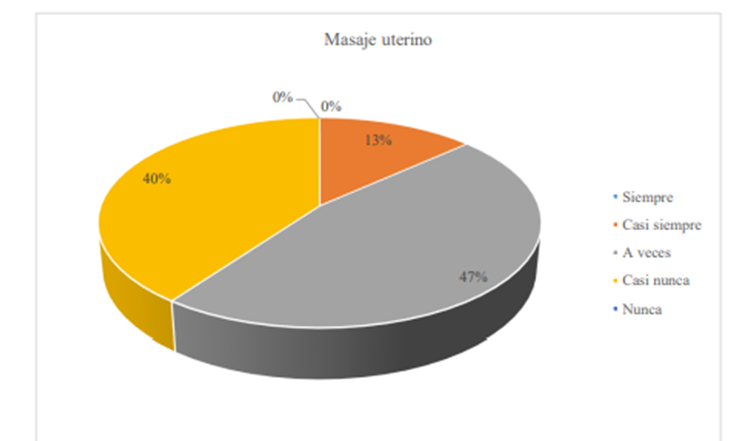
Source: Orrala et al.(25)
Figure 4. Uterine massage
CONCLUSIONS
About the research carried out, postpartum hemorrhage is the leading cause of maternal mortality in developing countries, and in Ecuador, it is the second leading cause of maternal death after hypertension disorders in pregnancy.
· Therefore, it has been shown that postpartum hemorrhage is a condition that causes maternal morbidity and mortality during childbirth. The most predominant nursing roles in this pathology are care and education, considering that from the first level of care, professional nursing staff carry out educational activities that provide pregnant women with knowledge about how to recognize the warning signs of postpartum hemorrhage. Similarly, as part of their care role, professional nurses are responsible for providing adequate care to patients suffering from this condition, through regular review of the regulations and protocols outlined in the Clinical Practice Guidelines issued by the Ecuadorian Ministry of Public Health.
· It was found that nursing professionals are responsible for providing adequate care to patients with postpartum hemorrhage, including constantly assessing the patient's vital signs every 15 minutes, maintaining a patent peripheral line and constant fluid flow to prevent hypovolemia, administering uterotonic drugs, correcting uterine atony, and performing uterine massage to evacuate clots, reviewing procedures such as blood transfusion in cases where patients warrant it, all under the application of the Nursing Care Process.
· The signs, symptoms, and behaviors presented by the patient in postpartum hemorrhage may vary. However, it is necessary to identify the most common ones, such as uncontrollable bleeding during expected delivery or cesarean section, which could lead to complications such as hypovolemic shock, altered blood pressure values, increased heart rate, decreased red blood cells, inflammation, and vaginal pain, among others.
· The nursing care process (NCP) is a tool that helps nurses improve their care methods and assess changes in patients. In postpartum hemorrhage, it is necessary to assess the patient to establish a nursing diagnosis and plan, execute, and evaluate activities, taking into consideration the primary diagnoses that may be assigned according to this pathology.
· Nursing professionals must continuously review the regulations established by the Ministry of Public Health, such as the Clinical Practice Guide for the Prevention, Diagnosis, and Treatment of Postpartum Hemorrhage, contributing to their ongoing training by providing appropriate care for patients in these health conditions.
RECOMMENDATIONS
Once this research has been carried out, it can be stated that postpartum hemorrhage is one of the leading causes of death in women, for which the following recommendations are established:
It is recommended that nursing staff provide care in the most efficient manner and according to the needs of the patients. It is essential for nursing professionals to continually monitor vital signs and accurately administer medications, ensuring their role is dynamic and tailored to the needs of patients.
When nursing professionals care for patients with this clinical condition of postpartum hemorrhage, it is recommended that they contribute to improving the quality of care provided by the staff. It is essential to consider international standards for managing massive obstetric hemorrhage, taking into account the severity of the clinical picture. For this reason, nursing staff must make an accurate diagnosis and activate the staff action protocol.
The nurse is responsible for maintaining direct contact with the patient at all times. For this reason, it is recommended that nurses receive the most efficient training and instruction possible for the early detection of postpartum hemorrhage. This requires knowledge of the most common signs and symptoms at the onset of postpartum hemorrhage. To this end, they must be familiar with the mechanism for activating the protocol established in each institution in the event of a case of massive hemorrhage, as well as the correct initial management of the condition.
Postpartum hemorrhage can be considered an emergency requiring immediate action, so healthcare professionals must have adequate training to act in these situations. Practical training enables professionals to internalize the sequence of actions to be taken and the ideal moment for each one, which is why it is essential to integrate theoretical knowledge into daily clinical practice.
Following the guidelines established by the Ministry of Public Health regarding the practical clinical guide for the prevention, diagnosis, and treatment of postpartum hemorrhage is essential for the proper treatment of these cases. It is therefore vital to keep in mind the massive hemorrhage protocols that emphasize the unequivocal identification of the patient, particularly when care is associated with a risk process, such as the transfusion of blood products in emergencies.
BIBLIOGRAPHIC REFERENCES
1. Pacheco JAC. La teoría Déficit de autocuidado: Dorothea Elizabeth Orem. Gac Méd Espirit. 2017;19(3):89-100. https://www.medigraphic.com/pdfs/espirituana/gme-2017/gme173i.pdf
2. Guachamín Peralvo PA, Díaz Rodríguez SA, Vásquez Orozco BJ, Churo Hidalgo VE, Chicango Ramírez RM, Yagual González BL, Páez Moreno JD. Cuidados de enfermería en pacientes con hemorragia digestiva que ingresan a la Unidad Técnica de Gastroenterología. Rev Méd-Cient CAMbios HECAM. 2020;19(1):132-43. https://doi.org/10.36015/cambios.v19.n1.2020.520
3. Tamayo JO. Hemorragia postpartum. Ginecol Obstet Mex. 2019;20(117):729-32. https://www.flasog.org/static/libros/Hemorragia-Postparto-17OCTUBRE.pdf
4. Organización Mundial de la Salud. Recomendaciones de la OMS para la prevención y el tratamiento de la hemorragia posparto. 2018. http://apps.who.int/iris/bitstream/handle/10665/141472/9789243548500_spa.pdf
5. Dandicourt C. El cuidado de enfermería con enfoque en la comunidad. Rev Cubana Med Gen Integr. 2018;34(1):55-62.
6. Alfaro L. Proceso de Atención de Enfermería (PAE). Salud Pública Paraguay. 2013;3:41-48. https://doi.org/10.1074/jbc.M112.419150
7. Onasis J, Llombar F, Sierra RE, Sucet K, Armas E, Joseff IB. Pospartum hemorrhage. Rev Cub Anestesiol Reanim. 2019;18(2):1-12. https://www.medigraphic.com/pdfs/revcubanerea/rca-2019/rca192c.pdf
8. Nava-Guerrero EN, Nungaray-González L, Salcedo A, Cisneros-Rivera F, Perales-Dávila J, Durán-Luna A. Morbilidad materna extrema: intervenciones médico-quirúrgicas e indicadores para evitar la muerte materna. Ginecol Obstet Mex. 2020;88(9):606-14. https://www.medigraphic.com/pdfs/ginobsmex/gom-2020/gom209f.pdf
9. Ministerio de Salud Pública del Ecuador. Prevención, diagnóstico y tratamiento de la hemorragia postparto. 2013. https://www.salud.gob.ec/wp-content/uploads/2016/09/Guía-de-hemorragia-postparto.pdf
10. Paccha Dueñas MV. Fisiopatología y tratamiento de la hemorragia postparto precoz. Universidad Central del Ecuador; 2020. http://www.dspace.uce.edu.ec/bitstream/25000/22472/1/T-UCE-0020-CDI-493.pdf
11. Benito D, Hurtado Moya D, Carmona D. Desgarros perineales postparto. Protocolos De Obstetricia Huvn. 2020;2019:1-5.
12. López-García LF, Ruiz-Fernández DP, Zambrano-Cerón CG, Rubio-Romero JA. Incidence of postpartum hemorrhage based on the use of uterotonics. Maternal outcomes in an intermediate complexity hospital in Bogotá, Colombia, 2016. Rev Colomb Obstet Ginecol. 2017;68(3):218-27. https://doi.org/10.18597/rcog.2916
13. Vázquez-Cruz E, Sotomayor-Tapia J, González-López AM, Montiel-Jarquín ÁJ, Gutierrez-Gabriel I, Romero-Figueroa MS. Patient satisfaction in primary medical care in Mexico. Rev Salud Publica. 2018;20(2):254-7. https://doi.org/10.15446/rsap.v20n2.61652
14. Voto L, Rivarola C. Postparto. ACTUALIZACIÓN DE CONSENSO DE OBSTETRICIA. Hemorragia Postparto. Federación Argentina de Sociedades de Ginecología y Obstetricia; 2019. http://www.fasgo.org.ar/archivos/consensos/Consenso_2019_Hemorragia_Post_Parto.pdf
15. López Martinez C. La hemorragia postparto: descripción, manejo y tratamiento. Universidad de Cantabria; 2017. https://repositorio.unican.es/xmlui/handle/10902/11759
16. Pazmiño Sánchez Y, Terán JO. Atención prehospitalaria de la hemorragia posparto inmediato. Rev Inv Acad Educ ISTCRE. 2017;1(2):13-8. https://www.revistaacademica-istcre.edu.ec/admin/postPDF/Atenciónprehospitalariadelahemorragiapospartoinmediato.pdf
17. Gilsanz Rodríguez F, Guasch Arévalo E, Brogly N, Alsina E, Puertas L, Domínguez A. Hemorragia obstétrica. Act En Anestesiol y Reanim. 2014;19(2):49-60. https://doi.org/10.1016/b978-84-8086-334-6.50140-1
18. Rizo Maradiaga J. Técnicas de investigación documental. Universidad Autónoma de Nicaragua; 2015. https://repositorio.unan.edu.ni/12168/1/100795.pdf
19. Sampieri H. Metodología de la investigación. 6th ed. McGraw-Hill; 2014. https://www.uca.ac.cr/wp-content/uploads/2017/10/Investigacion.pdf
20. Hernández Mendoza LD, Herrera Villalobos JE, Mendoza Hernández F, Adaya Leythe EA. Acretismo placentario: Experiencia en Obstetricia Crítica. Rev Méd Univ Veracruzana. 2018;18(1):75-87.
21. Sandra M. Factores de riesgo asociados con hemorragias postparto en pacientes atendidas en el Hospital de la Amistad Perú Corea II-2 Santa Rosa de Piura 2017. Universidad Nacional de Piura; 2019. https://repositorio.unp.edu.pe/bitstream/handle/UNP/1623/OBS-MOC-CHA-2018.pdf
22. Gomez N, Morillo J, Pilatuña C. El cuidado de enfermería en pacientes con atonía uterina atendidas en el hospital general Puyo de México. J Apl Tecnol Pangan. 2021;4(1):1-2. http://www.ejurnal.its.ac.id/index.php/sains_seni/article/view/10544
23. Margarita M, Esteban S, Cesar V, Mariela B. Factores asociados a la hemorragia obstétrica en el postparto inmediato: Hospital Juan Bruno Zayas. Soc Med Am. 2019;4(10):1-12. https://revistamedicasinergia.com/index.php/rms/article/view/269/622
24. Graciela R. Intervenciones de Enfermería durante la hemorragia postparto por atonía uterina. Universidad Nacional Autónoma de Nicaragua; 2020. http://repositorio.unan.edu.ni/2986/1/5624.pdf
25. Orrala E, Figueroa C. Cuidados de enfermería en pacientes con hemorragias postparto en el área de emergencia gineco-obstetricia. Hospital General Guasmo Sur, 2020. Universidad Estatal Península de Santa Elena; 2020. https://repositorio.upse.edu.ec/xmlui/bitstream/handle/46000/6014/UPSE-TEN-2021-0056.pdf
26. Bermejo M. Caso clínico: Plan de cuidados de enfermería estandarizado en hemorragia posparto. Benemérita Universidad Autónoma de Puebla; 2020. https://repositorioinstitucional.buap.mx/bitstream/handle/20.500.12371/12607/20210303122833-3989-T.pdf
27. Bruno J, Cuba S. Uso de las prostaglandinas. Medisan. 2017;19(1):113-21. http://scielo.sld.cu/pdf/san/v19n1/san15191.pdf
28. Bula J, Guzman M, Sanchez Á. Hemorragia posparto primaria en un hospital: characterization of maternal outcomes of primary postpartum. Hemorragia Postparto. 2017. https://revistas.unicordoba.edu.co/index.php/avancesalud/article/view/1392/1664
29. Castillo F. Guía de práctica clínica para prevención, diagnóstico y tratamiento de la hemorragia postparto. Hospital Cayetano Heredia; 2019. http://www.hospitalcayetano.gob.pe/PortalWeb/wp-content/uploads/resoluciones/2019/rd/RD_432-2019-HCH-DG.pdf
30. Clachar G. Hemorragia postparto precoz. Rev Méd Cienc Costa Rica. 2014;609:79-84. https://www.binasss.sa.cr/revistas/rmcc/609/art14.pdf
31. Columbié Fariñas T, Pérez Castillo R, Cordero Gonzalez Y. Factores asociados a la hemorragia obstétrica en el postparto inmediato: Hospital Juan Bruno Zayas. Rev Med Sinergia. 2019;4(10):e269. https://doi.org/10.31434/rms.v4i10.269
32. Conislla Y, Quispe E. Características sociodemográficas y obstétricas de puérperas que presentaron retención placentaria en el Centro de Salud de El Tambo 2017 y 2018. Universidad Nacional de Huancavelica; 2019. http://repositorio.unh.edu.pe/handle/UNH/2755
33. Cruz Cordova GC, Flores Nolasco MA. Guia De Atencion De. Ministerio de Salud del Perú; 2020. https://docs.bvsalud.org/biblioref/2020/11/1128238/28-11106280.pdf
34. Arco-Canoles ODC, Suarez-Calle ZK. Rol de los profesionales de enfermería en el sistema de salud colombiano. Univ Salud. 2018;20(2):171. https://doi.org/10.22267/rus.182002.121
35. Aldo S. Hemorragia del PostParto. Principales etiologías, su prevención, diagnóstico y tratamiento. Rev Med Clin Las Condes. 2017;10-12.
36. Aldo S. Principales etiologías, su tratamiento. Rev Med Clin Las Condes. 2018;25(6):993-1003.
37. Di Marco I, Davidson H, Fabiano P, Sar S. Consenso de Hemorragia Postparto/SOGIBA/2018. Sociedad de Obstetricia y Ginecología de Buenos Aires; 2018. http://www.sogiba.org.ar/images/Consenso_HPP_SOGIBA_2018.pdf
38. Diago Almela JV, Perales Puchalt A, Cohen MC, Perales Marín A. Muerte fetal tardía. En: Libro blanco de la muerte súbita infantil. Asociación Española de Pediatría; 2015. p. 29-36. https://www.aeped.es/sites/default/files/documentos/libro_blanco_muerte_subita_3ed_1382443264.pdf
39. García M. Hemorragia Postparto por inervación uterina. Universidad Técnica de Ambato; 2017. https://repositorio.uta.edu.ec/handle/123456789/19565
40. García MCL, Ramos JA. Hemorragia posparto. En: Ejercer La Medicina. 2018. p. 193-202. https://doi.org/10.2307/j.ctt21kk0w3.24
41. Garcia O. Manejo de la hemorragia postparto. Instituto Guatemalteco de Seguridad Social; 2016. https://www.igssgt.org/wp-content/uploads/images/gpc-be/ginecoobstetricia/GPC-BE%2046%20HPP.pdf
42. Hechavarría R, López G. Ley de maternidad gratuita y atención a la infancia. Organización Internacional del Trabajo; 2017. http://www.ilo.org/dyn/travail/docs/1729/LEY%20DE%20MATERNIDAD%20GRATUITA%20Y%20ATENCIÓN%20A%20LA%20INFANCIA.pdf
43. Hernández-Morales MA, García-de la Torre JI. Factores de riesgo de hemorragia obstétrica. Ginecol Obstet Mex. 2017;84(12):757-64. https://www.medigraphic.com/pdfs/ginobsmex/gom-2016/gom1612d.pdf
44. Ludmir J, Bolati H, Valencia C. Carbetocina en la prevención de hemorragia posparto. Federación Argentina de Sociedades de Ginecología y Obstetricia; 2016. http://www.fasgo.org.ar/images/Carbetocina_en_la_prevencion_de_hemorragia_posparto.pdf
45. García-Benavides JL, Ramírez-Hernández MA, Moreno-Cárcamo M, Alonso-Ramírez E, Gorbea-Chávez V. Hemorragia obstétrica postparto: propuesta de un manejo básico integral, algoritmo de las 3 «C». Rev Mex Anestesiol. 2018;41(Supl 1):190-4. http://www.medigraphic.com/rma
46. Moreno JAL. Inversión uterina. In: Modelamiento logístico para la producción sostenible de biocombustibles. 2019. p. 35-44. https://doi.org/10.2307/j.ctvckq8c2.6
47. Naranjo-Hernández Y, González-Hernández L, Sánchez-Carmenate M. Proceso Atención de Enfermería desde la perspectiva docente. Rev Arch Med Camagüey. 2018;22(6):831-42. https://www.medigraphic.com/pdfs/medicocamaguey/amc-2018/amc186n.pdf
48. Ortiz Arroyo R, Ortiz Galindo A, García Díaz F, García López A. Polihidramnios. Ginecol Obstet Mex. 2018;32(193):513-9. https://doi.org/10.1016/b978-84-458-1311-9.50079-3
49. Véliz F, Núñez A, Selman A. Acretismo placentario: Un diagnóstico emergente. Abordaje quirúrgico no conservador. Rev Chil Obstet Ginecol. 2018;83(5):513-26. https://doi.org/10.4067/s0717-75262018000500513
50. Weeks A. Postpartum haemorrhage. In: Maternal and Infant Deaths: Chasing Millennium Development Goals 4 and 5. Cambridge University Press; 2017. p. 85-98. https://doi.org/10.1017/CBO9781107784758.008
51. Tello García JG. Proceso de atención de enfermería con riesgo alto, por hemorragia post parto inmediato. Rev Cubana Enferm. 2018;27(3):20-9. http://repositorio.utmachala.edu.ec/bitstream/48000/10790/1/CHUCHUCA%20CAIMINAGUA%20MARITZA%20JACQUELINE.pdf
52. Savirón R. Prevención y tratamiento médico de la hemorragia postparto. Sociedad Española de Ginecología y Obstetricia; 2018. https://www.cuidamosdelamujer.es/es/profesionales/documentacion/presentaciones-cursos.ficheros/815891-2018%20DR%20SAVIRON%20TRATAMIENTO%20MEDICO.pdf
53. Smud R, Sermukslis B. Macrosomía. Protocols Medicina Maternofetal Hospital Clínic- Hospital Sant Joan De Déu- Universitat De Barcelona. 2019;41(3):171-3. https://medicinafetalbarcelona.org/protocolos/es/patologia-fetal/macrosomia.pdf
54. Susana M. Recomendaciones en el uso de uterotónicos en la cesárea. Sociedad Catalana de Anestesiología, Reanimación y Terapéutica del Dolor; 2013. http://www.scartd.org/sap/docs/obstetricia/Uterotonicos.pdf
55. Rodríguez MCB, Terceros LAC. Episiotomía: procedimiento a elección y no de rutina. Rev Cient Cienc Méd. 2017;17(2):53-7. http://www.scielo.org.bo/pdf/rccm/v17n2/v17n2_a11.pdf
56. Román-Soto J, Oyola-García A, Quispe-Ilanzo M. Factores de riesgo de hemorragia primaria posparto. Rev Cuba Med Gen Integr. 2019;35(1):1-12. http://scielo.sld.cu/pdf/mgi/v35n1/1561-3038-mgi-35-01-e718.pdf
57. Romero Merino CE, Santillán Briones CA. Factores desencadenantes y tratamiento de la hemorragia postparto secundaria a hipotonía uterina. Universidad de Guayaquil; 2020. http://repositorio.ug.edu.ec/bitstream/redug/52387/1/CD-3335%20ROMERO%20MERINO%2C%20CAROLINA%20ELIZABETH%3B%20SANTILLAN%20BRIONES%2C%20CESAR%20ALBERTO.pdf
58. López Cruz F, Del Rocío G, De P, Barragán R, Tapia Ibáñez EX, Christopher D. Choque hipovolémico. 2018;63:48-54. http://www.medigraphic.org.mx
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Bryan Enrique Jarrin Valarezo, Joselyn Katherine Arias Olmedo, Kathiusca Paola Echeverría Caicedo.
Data curation: Bryan Enrique Jarrin Valarezo, Joselyn Katherine Arias Olmedo, Kathiusca Paola Echeverría Caicedo.
Formal analysis: Bryan Enrique Jarrin Valarezo, Joselyn Katherine Arias Olmedo, Kathiusca Paola Echeverría Caicedo.
Drafting - original draft: Bryan Enrique Jarrin Valarezo, Joselyn Katherine Arias Olmedo, Kathiusca Paola Echeverría Caicedo.
Writing - proofreading and editing: Bryan Enrique Jarrin Valarezo, Joselyn Katherine Arias Olmedo, Kathiusca Paola Echeverría Caicedo.