doi: 10.56294/nds202381
ORIGINAL
Nursing care in hypertensive patients with cardiovascular risk attending a primary care facility in North Lima
Cuidados de enfermería en pacientes hipertensos con riesgo cardiovascular que acuden a un establecimiento de atención primaria en Lima Norte
David
Hugo Bernedo-Moreira¹ ![]() ,
Alfredo Giovanni Lazo-Barreda²
,
Alfredo Giovanni Lazo-Barreda² ![]() ,
Paul Espiritu-Martinez³
,
Paul Espiritu-Martinez³ ![]() ,
Juan Richar Villacorta Guzmán⁴
,
Juan Richar Villacorta Guzmán⁴ ![]() *, Ariel Sosa Remón⁵
*, Ariel Sosa Remón⁵ ![]()
¹Universidad Peruana Unión. Perú.
²Universidad Nacional de San Agustín de Arequipa. Perú.
³Universidad Nacional Autónoma Altoandina de Tarma, Junín. Perú.
⁴Escuela Militar de Ingeniería. Bolivia.
⁵Instituto Nacional de Oncología y Radiobiología, Habana. Cuba.
Cite as: Bernedo-Moreira DH, Lazo-Barreda AG, Espiritu-Martinez P, Villacorta Guzmán JR, Sosa Remón A. Nursing care in hypertensive patients with cardiovascular risk attending a primary care facility in North Lima. Nursing Depths Series. 2023; 2:81. https://doi.org/10.56294/nds202381
Submitted: 01-11-2022 Revised: 16-03-2023 Accepted: 10-10-2023 Published: 11-10-2023
Editor: Dra.
Mileydis Cruz Quevedo ![]()
Corresponding author: Juan Richar Villacorta Guzmán *
ABSTRACT
Cardiovascular risks are a consequence of high blood pressure and exist in people with hypertension, but if it is not properly controlled, the risks can increase. Therefore, the objective of this research is to determine the nursing care provided to hypertensive patients with cardiovascular risk who attend a primary care facility in northern Lima. This is a quantitative, descriptive, cross-sectional study with a population of 265 participants who responded to a questionnaire on sociodemographic aspects and the cardiovascular risk calculator. The results show that 4,2 % have very high cardiovascular risk, 10,9 % have high cardiovascular risk, 37,4 % have moderate cardiovascular risk, and 47,5 % have very low cardiovascular risk. In conclusion, people with high blood pressure should be educated about the risks that the disease can cause and how to minimize the risks that can affect their health and well-being.
Keywords: Hypertension; Cardiovascular Diseases; Heart Disease Risk Factors; Nursing Care.
RESUMEN
Los riesgos cardiovasculares son consecuencia de la hipertensión arterial existen en la persona que presenta hipertensión arterial, pero si no es controlada adecuadamente, los riesgos pueden aumentar, por ello, el objetivo de investigación es determinar los cuidados de enfermería en pacientes hipertensos con riesgo cardiovascular que acuden a un establecimiento de atención primaria en Lima Norte. Es un estudio cuantitativo, descriptivo-transversal, con una población de 265 participantes que respondieron un cuestionario de aspectos sociodemográficos y la calculadora de riesgo cardiovascular. En los resultados podemos observar que, el 4,2 % tiene riesgo cardiovascular muy alto, 10,9 % riesgo cardiovascular alto, 37,4 % riesgo cardiovascular moderado y 47,5 % riesgo cardiovascular muy bajo. En conclusión, se debe educar a la persona con hipertensión arterial sobre los riesgos que puede generar la enfermedad, y como minimizar los riesgos que pueden afectar su bienestar de salud.
Palabras clave: Hipertensión; Enfermedades Cardiovasculares; Factores de Riesgo de Enfermedades Cardíacas; Cuidados de Enfermería.
INTRODUCTION
Cardiovascular diseases (CVD) are a group of disorders of the heart and blood vessels and are the leading cause of death worldwide.(1) They appear to affect men and women differently, being the most common cause of death in women worldwide, even in developing countries.(2,3)
High blood pressure (HBP) is a condition characterized by blood pressure exceeding 140/90 mmHg. The estimated global prevalence is approximately one billion individuals, and around 7,1 million deaths per year could be attributed to HBP.(4) Suboptimal blood pressure (BP) is responsible for 62 % of cerebrovascular disease and 49 % of ischemic heart disease, with small variations due to gender.(5,6)
Deaths from cardiovascular disease have increased worldwide due to population growth, aging, and epidemiological changes.(7) In addition, cardiovascular disease is the leading cause of premature death and disability worldwide (myocardial infarction, cardiac death, and fatal or non-fatal stroke), accounting for more than 17 million deaths annually, mainly affecting people in low- and middle-income countries; It is estimated that 80 % of the global burden occurs in these countries.(8,9)
Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with a life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other physical, psychosocial, and spiritual problems.(10)
The potential benefits of primary prevention strategies based on studies are useful for verifying the reduction of cardiovascular disease events.(11) The harmful consequences of multiple risk factors are additive.(12,13)
A study conducted in Colombia (14) explains that cardiovascular disease remains the leading cause of death worldwide. Women have a protective factor against this during their reproductive years due to the effect of estrogen on the vascular endothelium, which is characteristic of this stage of life; subsequently, perimenopause and postmenopause lead to states of hypoestrogenemia that increase the risk of cardiovascular disease and death from this cause.
Another study conducted in Colombia (15) found that the average age of the population in the cardiovascular risk program was 38,11 years and the body mass index was 26,00 m2/kg. 7,58 % had high blood pressure, 1,08 % had diabetes mellitus, and 24,91 % were smokers. The cardiovascular risk calculated using the Framingham scale was 4,48 %. Body mass index, age, and systolic blood pressure are not statistically significant for risk assessment using the Framingham scale.
In a study conducted in Paraguay (16) the average age was 23 ± 4 years, most were from urban areas, 58 % were male, and had a low level of education. The mean body mass index was 23,5 ± 5 mm, and 58 % had no family history of hypertension. The mean blood pressure readings were 150 mmHg for systolic and 100 mmHg for diastolic. Secondary hypertension was detected in 86 % of the sample. The most common etiology was parenchymal kidney disease (86 %), of which 89 % had chronic kidney disease and lupus nephritis. The frequency of target organ damage was 86 %, the fundus was abnormal in 8 %, 46 % had left ventricular hypertrophy on electrocardiogram and 58 % on echocardiogram, 78 % had abnormal renal architecture on ultrasound, 57 % had elevated creatininuria, 76 % had traces of protein in random urine, and 80 % had elevated 24-hour proteinuria.
Therefore, the objective is to determine the nursing care required for hypertensive patients with cardiovascular risk who attend a primary care facility in northern Lima.
METHOD
Research type and design
In the respective research, according to its properties for data collection, it is quantitative in approach, with a non-experimental descriptive-transversal methodology.(17)
Population
The population consists of a total of 265 participants with high blood pressure.
Inclusion Criteria
· Participants who visit the health facility more than three times
· Participants who are over 18 years of age
· Participants who agree to participate voluntarily in the study
Technique and Instrument
The data collection technique will be a survey, which will include sociodemographic information and the PAHO cardiovascular risk calculator.
The cardiovascular risk calculator was developed by the PAHO GEDIC group. It includes the indicators listed below at : gender, age, tobacco use, maximum systolic blood pressure in mmHg, presence of diabetes, and total cholesterol in mg/dl. The final values produced by the calculator are: low risk <5 %, moderate risk 5 %-10 %, high risk 10 %-20 %, very high risk 20 %-30 %, and critical risk ≥30 %.(18)
Place and Application of the Instrument
To carry out the study, coordination was established with the head of the health facility and with the professionals in charge of the services where hypertensive patients are treated. Information about the research was also provided for their knowledge.
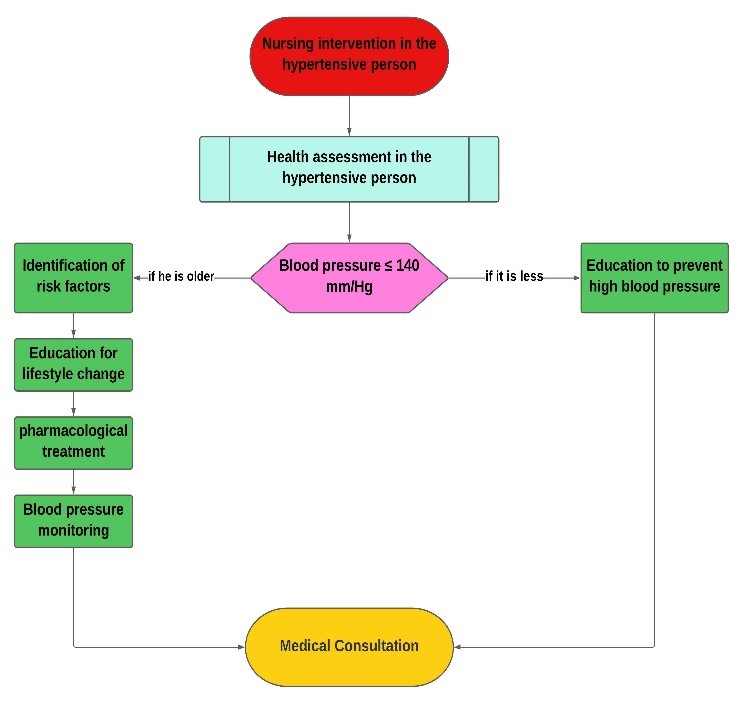
Figure 1. Flow chart of the intervention carried out by the nursing professional for the care of hypertensive patients
In this flow chart, we can see the intervention carried out by the nursing professional to then provide the necessary care to the hypertensive patient.
Hypertension is associated with cardiovascular problems, which depend on factors such as family and personal history, and can be determined through physical examination and laboratory tests.
The diagram shows that when the nurse observes that the blood pressure is greater than or less than 140 mm/Hg, they determine certain points at which they will minimize the risks that may compromise the hypertension.
If the pressure is higher than 140 mm/Hg, the nursing professional must carry out four important steps:
· Identify risk factors
· Educate the person with hypertension to modify their lifestyle
· Follow the medication prescribed by the primary care physician
· Monitor the blood pressure of the person with hypertension
If the pressure is less than 140 mm/Hg, the nursing professional must educate the person with HTN about the risks and complications that can contribute to the disease, given that the risk of cardiovascular problems increases due to HTN.
Once the nurse has completed the intervention, the person with HTN will be referred to their primary care physician for treatment according to the assessment of the person with HTN.
RESULTS
In figure 2, we can see that 47,5 % (n=126) of participants with hypertension have a very low cardiovascular risk, 37,4 % (n=99) have a moderate cardiovascular risk, 10,9 % (n=29) have a high cardiovascular risk, and 4,2 % (n=11) have a very high cardiovascular risk.
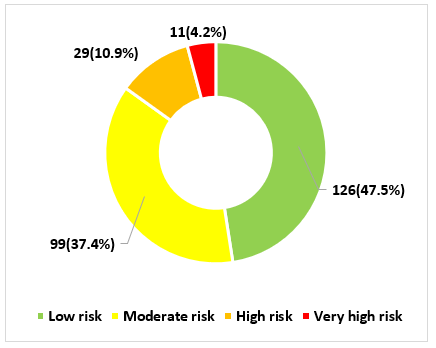
Figure 2. Cardiovascular risk in hypertensive patients attending a primary care facility in northern Lima
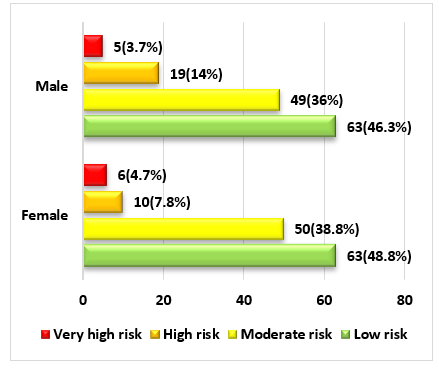
Figure 3. Cardiovascular risk in relation to sex in hypertensive patients attending a primary care facility in northern Lima
Figure 3 shows that, in relation to gender, 3,75 % (n=5) of males have a very high cardiovascular risk, 14 % (n=19) have a high cardiovascular risk, 36 % (n=49) have a moderate cardiovascular risk, and 46,3 % (n=63) have a low cardiovascular risk. and in females, 4,7 % (n=6) have a very high cardiovascular risk, 7,8 % (n=10) have a high cardiovascular risk, 38,8 % (n=50) have a moderate cardiovascular risk, and 48,8 % (n=63) have a low cardiovascular risk.
In figure 4, we can see that 59 % (n=95) of adult participants have a low cardiovascular risk, 35,4 % (n=57) have a moderate cardiovascular risk, 5,6 % (n=9) have a high cardiovascular risk, and none of the adults presented a very high cardiovascular risk. As for older adults, 29,8 % (n=31) have a low cardiovascular risk, 40,4 % (n=42) have a moderate cardiovascular risk, 19,2 % (n=20) have a high cardiovascular risk, and 10,6 % (n=11) have a very high cardiovascular risk.
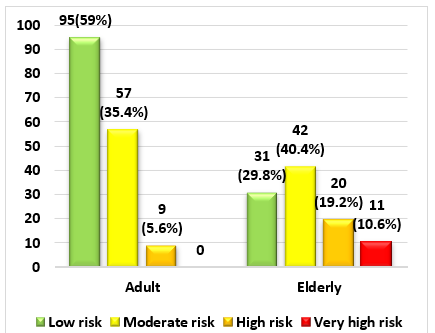
Figure 4. Cardiovascular risk in relation to age group in hypertensive patients attending a primary care facility in northern Lima
DISCUSSIONS
The current study was conducted from a public and community health perspective on the cardiovascular risks that can arise in people with high blood pressure, given that it is one of the diseases considered a health priority.
With regard to the cardiovascular risk results in hypertensive individuals, they have a low cardiovascular risk. This is because most hypertensive individuals are taking preventive measures to avoid other risks resulting from hypertension or other silent diseases. While it is true that factors that can increase cardiovascular risks in a hypertensive patient include unhealthy habits, such as an inadequate lifestyle, smoking, being overweight or obese, being sedentary, alcohol abuse, and non-modifiable characteristics such as age, sex, or family history. All of these factors can compromise hypertensive individuals, given that risks can arise without them realizing it and cause complications, since people under 60 with HTN have at least one cardiovascular risk factor and in those over 60, the factors tend to increase. However, people with HTN who adopt or maintain healthy habits keep their health in balance with the disease, preventing most cardiovascular risk factors from becoming apparent and allowing them to enjoy a good quality of life.
In terms of gender and age, we observe that they have a low cardiovascular risk. This is because healthy habits allow people with HTN to keep the disease stable and prevent risk factors that compromise their health from becoming evident. However, when a person does not have healthy habits, these risks can occur more regularly in males than in females, given that men are more prone to developing HTN due to not having healthy habits when they are young, a sedentary lifestyle, excessive tobacco and alcohol consumption, a lack of physical activity, and an inadequate diet. Over time, this leads to the development of the disease. In contrast, in women, blood pressure is low before reaching menopause, between the ages of 48 and 52. Cardiovascular risks and high blood pressure tend to be higher, given that the decrease in female hormones and estrogen are not the only causes of HTN in women. Other factors such as obesity, high cholesterol, or high triglycerides may also play a role.
CONCLUSIONS
It is concluded that strategies to promote awareness and prevent the risks associated with HTN should be considered so that people with this disease are aware of its potential consequences.
It is concluded that people with hypertension should be educated so that they can learn to take better care of themselves, allowing them to have a good quality of life and reduce the risks that may arise.
REFERENCES
1. Maharani A, Sujarwoto D, Oceandy D, Tampubolon G, Patel A. Cardiovascular disease risk factor prevalence and estimated 10-year cardiovascular risk scores in Indonesia: The Smarthealth Extend study. PLoS One. 2019;14(4):1-13. doi: http://10.1371/journal.pone.0215219.
2. Van L, Van Beers M, Kroes J, Van De Stadt L, Van Schaardenburg D, Nurmoham M. Cardiovascular risk in persons at risk of developing rheumatoid arthritis. PLoS One. 2020;15(8):1-11. doi: http://10.1371/journal.pone.0237072.
3. Abrams J, et al. Conocimientos de la hipertensión: Health beliefs about hypertension in an under-resourced community in the dominican republic. PLoS One. 2020;15(6):1-13. doi: http://10.1371/journal.pone.0235088.
4. Cuba M, Martinez J, Ortiz-Galeano I. Riesgo cardiovascular y uso adecuado de aspirina en prevención primaria de eventos cardiovasculares en el ambulatorio de Clínica Médica del Hospital de Clínicas. An Fac Cienc Med. 2020;53(2):53-58. http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S1816-89492020000200053.
5. Pajuelo J, Bernui I, Delgado D, Palomo P, Aquino A, Cochachin O. Riesgo cardiovascular en una población escolar con exceso de peso. An Fac Med. 2020;81(3):278-284. doi: http://10.15381/anales.v81i3.19603.
6. Suárez J, Gutiérrez M. Riesgo cardiovascular según la intensidad del climaterio en mujeres de edad mediana con antecedentes de preeclampsia. Rev Cient Medicentro (Villa Clara). 2020;24(3):531-547. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30432020000300531.
7. Paramio A, González L, Lasoncex D, Pérez E, Carrazana E. Riesgo cardiovascular global en el adulto mayor vinculado a los programas de actividad física comunitaria. CorSalud. 2020;12(3):318-326. http://www.revcorsalud.sld.cu/index.php/cors/article/view/464/1286.
8. Revueltas M, Valdés Y, Serra S, Suárez R, Ramírez J. Estimación del riesgo cardiovascular en una población, según dos tablas predictivas. Arch Méd Camagüey. 2020;24(5):668-700. http://www.revistaamc.sld.cu/index.php/amc/article/view/7533/3636.
9. Almazán M. Cardiovascular risk factors in young Mexican adults. Arch Cardiol Mex. 2020;90(4):427-435. doi: http://10.24875/ACM.20000258.
10. Expósito M. Palliative Care and Nursing: A Look Inside. Aquichan. 2022;22(2):1-4. doi: http://10.5294/aqui.2022.22.2.1.
11. García L, Centurión O. Medidas preventivas y manejo diagnóstico y terapéutico de la hipertensión arterial y las crisis hipertensivas. Rev Salud Publica Parag. 2020;10(2):59-66. http://scielo.iics.una.py/scielo.php?script=sci_arttext&pid=S2307-33492020000200059.
12. Kanna B, et al. Qualitative study of knowledge, perception, behavior and barriers associated with cardiovascular disease risk among overweight and obese Hispanic taxi drivers of South Bronx, NYC. BMC Public Health. 2020;20(1):1-10. doi: http://10.1186/s12889-020-08751-0.
13. Cerpa S, Rimarachín L, A B. Asociación entre nivel socioeconómico y riesgo cardiovascular en la población peruana. Rev Saude Publica. 2022;75(4):e20210278. doi: http://10.1590/0034-7167-2021-0278.
14. Hurtado L, Saldarriaga C, Jaramillo L, Hormaza M. Cardiovascular risk during menopause: gynecologist and cardiologist view. Rev Colomb Cardiol. 2022;29(1):7-15. doi: http://10.24875/RCCAR.21000101.
15. Velandia E, Vargas L, Vargas Ó, Benavidez H. Prevalence of obesity and cardiovascular risk in workers in the hydrocarbon area. Rev Colomb Cardiol. 2022;29(1):57-63. doi: http://10.24875/RCCAR.M22000118.
16. Quintana A, et al. Caracterización de la hipertensión arterial en adultos menores de 30 años de edad de un hospital del Paraguay. Rev Virtual Soc Parag. 2022;9(2):44-54.
17. Fernández C, Baptista P. Metodología de la Investigación. 2015;634. http://observatorio.epacartagena.gov.co/wp-content/uploads/2017/08/metodologia-de-la-investigacion-sexta-edicion.compressed.pdf.
18. Organización Mundial de la Salud, Organización Panamericana de la Salud. Calculadora Riesgo Cardiovascular. OPS. 2007. https://www.paho.org/cardioapp/web/#.
FUNDING
None.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTION
Conceptualization: David Hugo Bernedo-Moreira, Alfredo Giovanni Lazo-Barreda, Paul Espiritu-Martinez, Juan Richar Villacorta Guzmán, Ariel Sosa Remón.
Research: David Hugo Bernedo-Moreira, Alfredo Giovanni Lazo-Barreda, Paul Espiritu-Martinez, Juan Richar Villacorta Guzmán, Ariel Sosa Remón.
Methodology: David Hugo Bernedo-Moreira, Alfredo Giovanni Lazo-Barreda, Paul Espiritu-Martinez, Juan Richar Villacorta Guzmán, Ariel Sosa Remón.
Writing – original draft: David Hugo Bernedo-Moreira, Alfredo Giovanni Lazo-Barreda, Paul Espiritu-Martinez, Juan Richar Villacorta Guzmán, Ariel Sosa Remón.
Writing – review and editing: David Hugo Bernedo-Moreira, Alfredo Giovanni Lazo-Barreda, Paul Espiritu-Martinez, Juan Richar Villacorta Guzmán, Ariel Sosa Remón.